Proactive Approaches to Effectively Manage High Blood Pressure
Managing high blood pressure is critical for ensuring long-term health and preventing serious complications associated with this widespread condition. Millions globally face the challenges of high blood pressure, also known as hypertension, often unaware of the severe risks it poses. Hypertension develops when blood consistently exerts excessive force against the arterial walls, leading to potential damage to blood vessels and significant strain on the heart. If not properly managed, this condition can result in grave consequences like heart disease, stroke, and kidney failure. Therefore, understanding your blood pressure readings and identifying contributing factors is essential for effective management.
Having a genetic predisposition can increase your risk of developing hypertension. If there is a family history of high blood pressure, you may find yourself at a greater risk of experiencing it in your lifetime. However, lifestyle decisions play an equally vital role in this equation. Diets high in salt, low in fruits and vegetables, and excessive alcohol intake can all heighten your risk for hypertension. A lack of physical activity and weight gain further exacerbate rising blood pressure levels. In today's fast-paced world, unhealthy habits have made hypertension increasingly prevalent. Nonetheless, by raising awareness and adopting proactive health strategies, individuals can significantly improve their health outcomes.
Many people suffering from high blood pressure often do not show any clear symptoms, which is why hypertension is frequently dubbed the “silent killer.” Relying solely on symptoms to gauge your health can lead to misleading assessments. Regular monitoring and health evaluations are vital for truly understanding your blood pressure levels. Given that readings can vary, consistent monitoring is essential for effective management. Upon being diagnosed with hypertension, implementing straightforward lifestyle changes can produce significant benefits. Increasing your level of physical activity, making healthier dietary choices, and applying effective stress management techniques can greatly lower your blood pressure and improve your overall health. If these lifestyle changes prove inadequate, discussing appropriate medication options with a healthcare provider may be necessary.
Successful management of high blood pressure requires a comprehensive approach that includes adopting healthy lifestyle habits, meticulous monitoring, and medication when required. This thorough strategy significantly mitigates the risk of developing severe health complications. The sooner you take control of your heart health, the better your outcomes will be. Through active engagement in managing hypertension, you can greatly enhance your quality of life now and in the years to come.
Enhancing Understanding of High Blood Pressure: Why It Matters
High blood pressure, known in medical terms as hypertension, signifies that your blood pressure consistently exceeds healthy levels. Blood pressure is measured in millimeters of mercury (mmHg) with two values: systolic (the pressure during heartbeats) and diastolic (the pressure between heartbeats). A healthy blood pressure reading is generally around 120/80 mmHg, while readings above 130/80 mmHg often indicate some form of hypertension.
Hypertension is primarily divided into two categories. Primary hypertension develops gradually and is often influenced by both genetic and lifestyle factors. On the other hand, secondary hypertension can occur due to other medical conditions, such as kidney disease or hormonal imbalances. Both forms of hypertension exert significant pressure on the heart and arteries, posing risks of kidney damage and negatively impacting cognitive abilities. Identifying the specific type of hypertension you have is crucial for effective management and treatment.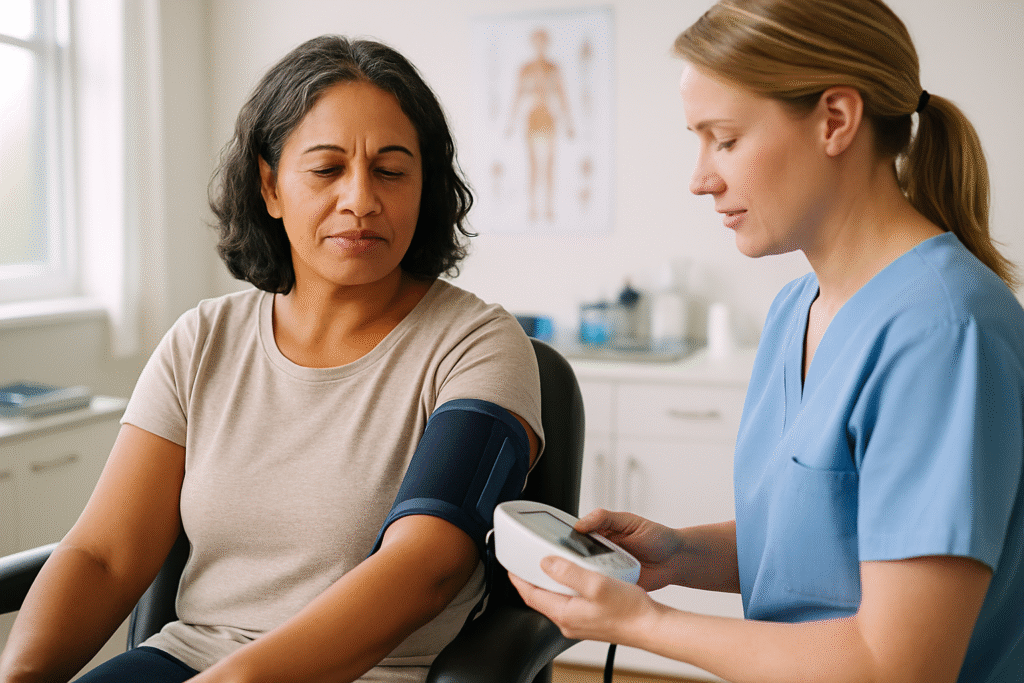
Managing high blood pressure often necessitates significant adjustments to daily routines and a close collaboration with healthcare providers. Many individuals are unaware of their hypertension, as symptoms rarely appear. This highlights the importance of regular health check-ups, as early detection allows for timely intervention before complications arise. Dietary changes, increased physical activity, and stress management techniques may be integral to effectively lowering blood pressure and improving quality of life.
By staying informed and proactive, you can protect your heart, brain, and kidneys. Managing high blood pressure is a lifelong commitment that can lead to improved health and greater peace of mind.
Identifying Key Contributors to Hypertension: Understanding the Causes
Numerous factors contribute to the onset of high blood pressure, broadly classified as genetic, lifestyle, and environmental influences. Genetic predisposition plays a pivotal role; individuals with a family history of hypertension are often more likely to develop the condition themselves. This hereditary aspect suggests specific biological mechanisms may predispose certain individuals to high blood pressure.
 Lifestyle choices also significantly affect the risk of developing hypertension. Diets excessively high in sodium can result in water retention, which increases blood volume and subsequently elevates blood pressure. Conversely, diets rich in potassium can help mitigate blood pressure levels. Foods like fruits and vegetables are excellent sources of potassium, essential for counteracting the adverse effects of excessive sodium by promoting relaxation in blood vessel walls. Moreover, a sedentary lifestyle further increases the risk of hypertension. Extended periods of inactivity often lead to weight gain, placing additional strain on the heart and arteries, ultimately resulting in higher blood pressure over time.
Lifestyle choices also significantly affect the risk of developing hypertension. Diets excessively high in sodium can result in water retention, which increases blood volume and subsequently elevates blood pressure. Conversely, diets rich in potassium can help mitigate blood pressure levels. Foods like fruits and vegetables are excellent sources of potassium, essential for counteracting the adverse effects of excessive sodium by promoting relaxation in blood vessel walls. Moreover, a sedentary lifestyle further increases the risk of hypertension. Extended periods of inactivity often lead to weight gain, placing additional strain on the heart and arteries, ultimately resulting in higher blood pressure over time.
Excessive alcohol consumption and smoking are well-documented contributors to hypertension. Heavy drinking significantly raises blood pressure, with risks escalating in proportion to the quantity consumed. Smoking harms the heart by damaging blood vessel walls and reducing their elasticity. This loss of flexibility can lead to increased blood pressure levels. Additionally, stress and poor sleep hygiene are recognized risk factors that can progressively elevate blood pressure. Fast-paced urban living often exacerbates these stressors, compromising mental health and potentially worsening hypertension.
Understanding these fundamental causes is crucial for effectively preventing and managing high blood pressure. By adopting healthier lifestyle choices and remaining vigilant about personal risk factors, individuals can significantly reduce their likelihood of developing hypertension. Knowledge is indeed a powerful ally in the fight against this pervasive condition.
Diagnosing Hypertension: Recognizing Symptoms and Testing Methods
High blood pressure is commonly referred to as “the silent killer” due to its lack of obvious symptoms. Most individuals with hypertension do not notice any significant signs until considerable damage has already occurred. This absence of symptoms emphasizes the necessity for regular monitoring. Without consistent evaluations, high blood pressure may go unnoticed, leading to severe health complications such as heart attacks or strokes.
Some individuals may occasionally experience symptoms such as headaches, shortness of breath, or nosebleeds, but these typically only occur when blood pressure reaches dangerously high levels. Because hypertension often presents without symptoms, healthcare professionals advocate for routine blood pressure screenings. It is especially critical for individuals over 40 or those with risk factors like obesity, inactivity, or a family history of heart disease to have their blood pressure assessed regularly.
Diagnosis typically involves measuring blood pressure with a sphygmomanometer in a clinical environment, comparing readings against established standards. Consistently elevated readings above 130/80 mmHg usually result in a hypertension diagnosis. After diagnosis, further evaluations may be necessary to exclude secondary causes of high blood pressure and assess overall cardiovascular health.
Recognizing the importance of early diagnosis empowers individuals to take proactive steps in managing their hypertension. With the right knowledge and resources, those at risk can implement lifestyle changes or seek medical assistance to protect their long-term health.
Holistic Strategies for Effectively Managing High Blood Pressure
Managing high blood pressure successfully necessitates a holistic strategy that blends lifestyle modifications, potential medication, and ongoing monitoring. The encouraging news is that many individuals can maintain healthy blood pressure levels through lifestyle changes alone. Regular physical activity, such as brisk walking or cycling, is critical for sustaining a healthy weight and enhancing cardiovascular health. Aim for at least 150 minutes of moderate aerobic exercise each week.
Diet is also a key element in effective blood pressure management. Embracing a balanced diet is essential for reducing blood pressure. The ideal diet should be low in saturated fats, cholesterol, and sodium while being rich in fruits, vegetables, whole grains, and lean proteins. The DASH diet (Dietary Approaches to Stop Hypertension) is a well-respected approach focusing on heart-healthy foods that assist in lowering blood pressure. Nutrients such as potassium, magnesium, and calcium are crucial for its effectiveness.
Incorporating stress management techniques such as yoga, meditation, and mindfulness can significantly influence blood pressure levels. Chronic stress is recognized as a contributing factor to elevated readings, making relaxation strategies an essential component of a holistic approach to hypertension management. Individuals must also be mindful of their alcohol and tobacco consumption, as both can exacerbate high blood pressure.
If lifestyle modifications prove insufficient, healthcare providers may recommend medications to help manage hypertension. These can include diuretics, ACE inhibitors, beta-blockers, and more. Regular blood pressure monitoring is essential, as it enables individuals and their healthcare providers to assess the effectiveness of management strategies and make necessary adjustments.
Taking a proactive approach to managing high blood pressure can lead to improved health outcomes and a reduced risk of complications. With the right strategies in place, individuals can take charge of their cardiovascular health and enjoy fulfilling lives.
The Role of Dietary Supplements in Blood Pressure Management
Navigating the complexities of hypertension management often prompts individuals to explore the potential benefits of dietary supplements. While supplements should not substitute a healthy lifestyle or prescribed medications, they can serve as valuable adjuncts in blood pressure management when integrated into a holistic approach. Supplements can offer essential nutrients that bolster cardiovascular health, making them an appealing option for those looking to enhance their overall well-being.
Certain supplements have garnered attention for their potential to help maintain healthy blood pressure levels. For instance, magnesium, potassium, and omega-3 fatty acids are frequently cited for their positive impacts on heart health. These nutrients may promote blood vessel relaxation, counteract sodium's effects, and reduce inflammation, respectively. However, it is vital to approach supplementation with a clear understanding of its limitations.
While dietary supplements can enhance overall health, they should not be viewed as a cure-all for hypertension. Relying solely on supplements without simultaneously implementing healthy lifestyle changes can result in missed opportunities for improving blood pressure management. Dietary modifications and regular physical activity should form the foundation of any plan to manage high blood pressure. Supplements can provide support, but they should complement—not replace—these core strategies.
Before embarking on any supplement regimen, it is crucial to consult healthcare providers. Each individual's health needs are unique, and a healthcare professional can offer guidance on safe and appropriate options. Collaborating with healthcare providers empowers individuals to make informed supplement choices, ensuring their selections align with their health goals and assist in better blood pressure control while minimizing the risk of complications.
Understanding the Role of Supplements in Managing High Blood Pressure
Supplements can significantly aid in blood pressure management, especially when integrated into a comprehensive dietary and lifestyle modification plan. Specific vitamins, minerals, and fatty acids have shown promise in promoting cardiovascular health and may assist in regulating blood pressure levels. For individuals managing hypertension, exploring suitable supplements can be an empowering step toward enhanced health.
Unlocking the Benefits of Magnesium for Blood Pressure Control
One of the most extensively researched supplements is magnesium. This essential mineral is renowned for its ability to relax blood vessels, potentially resulting in lower blood pressure levels. Studies indicate that adequate magnesium intake can help maintain blood pressure within a healthy range, particularly for individuals diagnosed with hypertension. Foods rich in magnesium, such as leafy greens, nuts, and whole grains, are valuable additions to any diet. However, many individuals struggle to obtain sufficient magnesium through food alone, making magnesium supplementation advantageous.
Potassium is another essential nutrient for regulating blood pressure. This mineral assists in balancing sodium levels in the body, thereby lowering overall blood pressure. Supplementation can be particularly beneficial for individuals who do not consume enough potassium-rich foods, such as bananas, avocados, and sweet potatoes. Maintaining an ideal potassium-to-sodium balance is crucial for supporting healthy blood pressure levels, making potassium supplementation an attractive option for many.
Omega-3 fatty acids, commonly sourced from fatty fish, walnuts, and flaxseeds, are well-known for their anti-inflammatory properties. Research has demonstrated that omega-3 supplementation can lead to modest reductions in blood pressure, making it a valuable addition for individuals aiming to manage hypertension. The heart-healthy advantages of omega-3s extend beyond merely regulating blood pressure, positively contributing to overall cardiovascular health and wellness.
Personalized Approaches: Tailoring Supplement Strategies for Hypertension
Supplements can support the management of high blood pressure when combined with healthy lifestyle changes. Incorporating magnesium, potassium, and omega-3 fatty acids into your routine may enhance heart health. It is crucial to align supplements with your individual health needs. Always consult a healthcare professional before starting any new supplement regimen.
Recognizing the Limitations of Supplements in Hypertension Management
Despite their potential benefits, it is essential to acknowledge the limitations of supplements in managing high blood pressure. While certain nutrients may enhance cardiovascular health, supplements should not be viewed as standalone solutions or substitutes for a balanced diet and healthy lifestyle choices. Over-reliance on supplements can lead to complacency regarding the essential lifestyle modifications necessary for effectively managing hypertension.
The quality, potency, and effectiveness of supplements can vary greatly, making it crucial for consumers to select reputable brands. Not all supplements are created equal; some may contain ingredients that interact with medications or may not be adequately absorbed by the body. Furthermore, excessive consumption of specific supplements can lead to adverse effects. For example, high doses of potassium supplementation can induce hyperkalemia, a potentially dangerous condition for individuals with kidney issues.
Supplements Can Assist But Shouldn't Replace Healthy Habits
The effectiveness of supplements can differ widely among individuals. Health conditions, genetics, and lifestyle factors all play a role in determining their efficacy. What benefits one person may not yield the same results for another. It is essential to have realistic expectations: supplements are merely one component of a broader blood pressure management strategy. They do not replace lifestyle changes or medical care. Consider supplements as helpful tools—not standalone solutions. A balanced diet, regular exercise, and prescribed medication may also be necessary components of an effective management plan.
Consult your healthcare provider before introducing any new supplements. This precaution helps you avoid harmful interactions or unnecessary risks. Your doctor can guide you toward choices that align with your health needs. A well-rounded plan is most effective. Combining healthy habits with expert advice offers the most reliable method for controlling blood pressure, thereby supporting long-term heart health.
The Importance of Consulting Healthcare Providers Before Supplementation
Before initiating any supplement regimen, it is crucial to engage in discussions with healthcare providers. Each individual's health profile is distinct, meaning dietary requirements and potential interactions with medications can vary significantly. A healthcare provider can thoroughly evaluate one's health status and offer tailored recommendations, ensuring that any supplementation strategy aligns with overall health goals.
Consultation with healthcare professionals is particularly vital for those already managing chronic conditions or taking medications for hypertension. Certain supplements may interact with prescribed blood pressure medications, potentially leading to adverse effects or diminished treatment efficacy. For example, potassium supplements may pose complications for individuals on specific antihypertensive medications, underscoring the necessity for professional guidance before introducing new supplements.
Understanding the potential risks and benefits of supplementation is essential. Not all supplements undergo the same level of scrutiny as prescription medications, which can lead to variability in quality and potency. Healthcare providers can recommend high-quality products and help identify reputable brands that undergo third-party testing for safety and efficacy.
Regular follow-ups with healthcare providers ensure that individuals maintain open lines of communication regarding their health status and any changes in their supplement regimen. This ongoing relationship allows for necessary adjustments based on blood pressure readings and overall health progress. An informed approach to supplementation, guided by healthcare expertise, can empower individuals to take an active role in managing their blood pressure and enhancing overall health outcomes.
Effective Supplements for Supporting High Blood Pressure Management
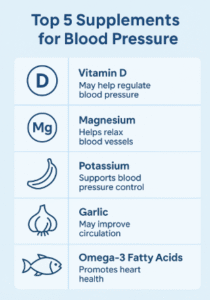
Several supplements have gained recognition for their potential efficacy in managing high blood pressure effectively. Among these, magnesium, potassium, and omega-3 fatty acids are standout options due to their well-documented benefits for cardiovascular health. Understanding the roles of these supplements can empower individuals to make informed decisions about their hypertension management strategies.
Magnesium: The Mineral That Supports Blood Vessel Relaxation
Magnesium is an essential mineral involved in numerous biochemical processes within the body. It plays a crucial role in muscle and nerve function, energy production, and maintaining normal blood pressure. Research indicates that magnesium supplementation can significantly lower blood pressure in individuals with hypertension, particularly among those with low dietary intake. Foods rich in magnesium, such as spinach, almonds, and black beans, are excellent choices; however, many individuals require supplements to meet their daily magnesium needs.
Potassium: Balancing Sodium Levels for Heart Health
Potassium is another vital nutrient that regulates blood pressure. By counteracting sodium's effects, potassium helps to relax blood vessel walls, thereby decreasing blood pressure. High-potassium foods, such as bananas, sweet potatoes, and leafy greens, are excellent choices for those seeking to manage hypertension. Supplementation can be beneficial for individuals who may not consume sufficient potassium through their diet, but it must be approached with caution, particularly for those with kidney issues.
Omega-3 Fatty Acids: Anti-Inflammatory Support for Heart Health
Omega-3 fatty acids, primarily derived from fatty fish such as salmon and mackerel, have been extensively researched for their cardiovascular benefits. These healthy fats reduce inflammation and improve endothelial function, thereby lowering blood pressure. Supplementation with omega-3 fatty acids has shown promise in modestly decreasing blood pressure levels, making them a valuable addition to a heart-healthy lifestyle. Fish oil or algal oil supplements can provide a convenient alternative for individuals who do not regularly consume fish. Incorporating these popular supplements into a broader strategy that includes a balanced diet and regular exercise can help individuals manage their blood pressure effectively. However, it is crucial to approach supplementation mindfully and consult with healthcare professionals to ensure safety and efficacy.
Investigating the Benefits of Coenzyme Q10 in Blood Pressure Management
Coenzyme Q10, often abbreviated as CoQ10, is a powerful antioxidant that plays a crucial role in cellular energy production. This compound has garnered attention for its potential benefits in lowering blood pressure, making it an appealing option for individuals seeking to manage hypertension. Exploring the benefits, dosage recommendations, and evidence supporting CoQ10’s role in blood pressure management can empower individuals to make informed decisions about their health.
Examining CoQ10’s Impact on Blood Pressure Control
CoQ10 is essential for the proper functioning of cells, particularly in the heart and blood vessels. Its antioxidant properties help reduce oxidative stress, which can damage blood vessels and contribute to elevated blood pressure levels. CoQ10 may assist in lowering blood pressure in individuals with hypertension by improving endothelial function and blood flow.
Research indicates that CoQ10 supplementation can lead to modest reductions in blood pressure, particularly among individuals diagnosed with hypertension. Some studies have reported decreases of 10-17 mmHg in systolic blood pressure and 5-10 mmHg in diastolic blood pressure among those taking CoQ10 supplements. These findings suggest that CoQ10 could be a valuable addition to a comprehensive hypertension management plan.
Additionally, CoQ10 may offer benefits beyond its effects on blood pressure. Its role in promoting heart health and improving energy production can enhance overall well-being. Individuals with cardiovascular disease or those taking statin medications, which can deplete CoQ10 levels, may particularly benefit from supplementation.
Incorporating CoQ10 into a holistic approach to managing hypertension can provide individuals with a natural option for supporting cardiovascular health. However, it is essential to consult a healthcare provider before supplementation, as individual needs vary significantly.
Determining Optimal Dosage and Safety Considerations for CoQ10
When considering CoQ10 supplementation, determining the appropriate dosage is vital for maximizing its benefits while minimizing potential side effects. Typical doses of CoQ10 range from 100 to 200 mg per day, although some studies have employed higher doses with positive outcomes. Consulting with a healthcare provider is crucial to establish the optimal dosage based on individual health profiles and goals.
CoQ10 is generally regarded as safe for most individuals, with few reported side effects. Some may experience mild gastrointestinal discomfort, headaches, or dizziness, but these effects are typically transient. Individuals taking certain medications, such as blood thinners, should consult their healthcare provider before commencing CoQ10, as it may interact with these medications.
Monitoring the effects of CoQ10 supplementation is crucial, especially for individuals managing hypertension. Regular blood pressure checks can help assess the supplement's effectiveness and guide any necessary dosage adjustments. By collaborating closely with healthcare providers, individuals can ensure their CoQ10 regimen is safe and effective.
Incorporating CoQ10 into a comprehensive hypertension management strategy can promote cardiovascular health and support overall well-being. With careful attention to dosage and safety, CoQ10 may offer a valuable addition to the toolkit for managing high blood pressure.
Research Findings: Evidence Supporting CoQ10 and Blood Pressure
The research surrounding CoQ10 and its role in blood pressure management is promising, although further studies are needed to establish definitive conclusions. Various clinical trials have investigated the effects of CoQ10 supplementation on blood pressure levels, with many reporting positive outcomes. For instance, a meta-analysis of multiple studies found that CoQ10 supplementation led to significant reductions in both systolic and diastolic blood pressure among individuals with hypertension.
While the findings are encouraging, it is crucial to recognize the variability in individual responses to CoQ10 supplementation. Some individuals may experience more pronounced reductions in blood pressure than others, depending on factors such as baseline levels, overall health, and adherence to a comprehensive management plan. Additionally, the duration of supplementation and the specific formulations used can influence results.
As interest in complementary therapies expands, ongoing research into CoQ10's long-term effects on blood pressure and cardiovascular health will be essential. Individuals contemplating CoQ10 should remain informed about emerging findings and consult their healthcare providers for guidance on the most effective strategies for managing their hypertension.
CoQ10 presents a promising option for those seeking natural ways to manage high blood pressure and enhance cardiovascular health. By understanding the benefits, dosage considerations, and current evidence, individuals can make informed decisions about integrating CoQ10 into their health regimen.
Harnessing the Power of Garlic for Blood Pressure Management
Garlic, a widely used culinary ingredient, has long been recognized for its potential health benefits, particularly in the realm of cardiovascular health. Research indicates that garlic may significantly lower blood pressure, making it a compelling option for individuals seeking natural solutions for hypertension management. Understanding how garlic works, the various forms and dosages available, and the clinical evidence supporting its use can empower individuals to make informed decisions about their health.
Mechanisms Behind Garlic’s Health Benefits
Garlic contains an active compound known as allicin, which is responsible for many of its health-promoting properties. Allicin has been shown to exert a vasodilatory effect, meaning it helps relax blood vessels and enhance blood flow. This relaxation of blood vessels can lead to lower blood pressure levels, making garlic a valuable addition to the diet for individuals managing hypertension.
In addition to its vasodilatory effects, garlic may possess anti-inflammatory and antioxidant properties, which can further contribute to cardiovascular health. By reducing oxidative stress and inflammation within the body, garlic may help protect against damage that can lead to elevated blood pressure levels.
Several studies have examined the effects of garlic on blood pressure, with numerous reports indicating positive outcomes. Research suggests that regular garlic consumption may lead to modest reductions in both systolic and diastolic blood pressure, particularly in individuals with hypertension. These findings underscore garlic's potential as a natural remedy for managing high blood pressure.
Incorporating garlic into a heart-healthy diet can provide numerous benefits beyond just blood pressure management. As a versatile ingredient, it can enhance the flavor of various dishes while promoting overall health. For those seeking natural alternatives to pharmaceuticals, garlic may serve as a valuable addition to their dietary regimen.
Exploring Garlic Forms and Dosages: Making Informed Choices
Garlic supplements are available in various forms, including capsules, tablets, and extracts. Each form may exhibit different bioavailability, affecting how well the body absorbs and utilizes the active compounds. Aged garlic extract, in particular, has gained popularity due to its high concentration of beneficial compounds and is often used for its potential health benefits.
The appropriate dosage of garlic for blood pressure management can vary based on the form used and the concentration of active ingredients. Generally, studies have employed doses ranging from 600 to 1,200 mg of garlic extract daily, while whole garlic cloves may require higher quantities to achieve similar effects. Consulting with a healthcare provider is crucial to determining the most suitable dosage tailored to individual health needs and goals. While garlic is generally considered safe for most individuals, it may lead to side effects such as bad breath or gastrointestinal discomfort. Garlic can interact with certain medications, particularly blood thinners, so consult a healthcare provider before supplementing.
Incorporating garlic into one’s diet, whether through whole cloves or supplements, can support heart health and aid in blood pressure management. By understanding the various forms and dosages available, individuals can make informed choices about how best to integrate this potent ingredient into their health regimen.
Clinical Evidence Supporting Garlic's Efficacy
A growing body of research supports the potential benefits of garlic for lowering blood pressure. Numerous clinical studies have investigated the effects of garlic supplementation on individuals with hypertension, with many reporting significant results. For instance, a meta-analysis published in the journal Hypertension found that garlic supplementation led to notable reductions in both systolic and diastolic blood pressure among participants, particularly those with higher baseline levels.
While the results are promising, it is essential to recognize that individual responses to garlic supplementation can vary widely. Some studies have shown more substantial blood pressure reductions, while others have reported minimal effects. Factors such as dosage, duration of supplementation, and individual health profiles can influence the outcomes of these studies.
The type of garlic used in supplementation can also impact results. Aged garlic extracts have been shown to possess higher bioavailability and may be more effective than fresh garlic or other forms. As research continues to explore the relationship between garlic and blood pressure management, individuals should remain informed about emerging findings and consult healthcare providers for guidance.
Incorporating garlic into a heart-healthy diet can provide numerous benefits, particularly for those managing high blood pressure. With the potential to support cardiovascular health, garlic is a natural option for individuals seeking alternatives to pharmaceutical interventions.
Awareness of Potential Side Effects and Interactions with Garlic
While garlic is generally safe for most individuals, it is essential to be aware of potential side effects and medication interactions. Common side effects of garlic supplementation include gastrointestinal discomfort, heartburn, and bad breath. These effects can often be mitigated by taking garlic supplements with food or opting for enteric-coated formulations.
Garlic can also interact with certain medications, particularly anticoagulants and antiplatelet drugs. This interaction may elevate the risk of bleeding, making it vital for individuals taking these medications to consult with a healthcare provider before starting garlic supplementation. Garlic may also affect the metabolism of certain drugs, altering their efficacy.
For individuals with specific health conditions, such as bleeding disorders or gastrointestinal issues, caution is advised when considering garlic supplementation. Consulting with a healthcare provider can provide valuable insights into potential risks and help determine whether garlic is suitable for blood pressure management.
In summary, while garlic offers numerous health benefits, individuals should approach supplementation mindfully, considering potential side effects and interactions. By consulting healthcare professionals, individuals can safely incorporate garlic into their hypertension management strategies and enjoy its cardiovascular benefits.
Investigating the Connection Between Vitamin D and Hypertension
Vitamin D, commonly referred to as the “sunshine vitamin,” is vital for overall health, including its potential influence on blood pressure regulation. Emerging research indicates that vitamin D deficiency may be linked to hypertension, making it essential for individuals to understand this critical nutrient's role in blood pressure management. By exploring the relationship between vitamin D and hypertension, individuals can proactively support their cardiovascular health.
Unpacking Vitamin D's Role in Blood Pressure Regulation
Vitamin D is a fat-soluble vitamin sourced from sunlight exposure, dietary intake, and supplements. It is essential for maintaining healthy bones and teeth, enhancing immune function, and regulating various physiological processes. Recent studies have examined the connection between vitamin D levels and hypertension, suggesting that adequate vitamin D may be instrumental in sustaining healthy blood pressure levels.
Research indicates that individuals with low vitamin D levels are at an increased risk of developing hypertension. The exact mechanisms underlying this relationship are still being explored, but it is believed that vitamin D may influence blood pressure through its effects on calcium metabolism, inflammation, and the renin-angiotensin-aldosterone system, which is a key regulator of blood pressure.
While the evidence linking vitamin D deficiency to hypertension is compelling, it is crucial to recognize that not all individuals with low vitamin D levels will develop high blood pressure. However, ensuring sufficient vitamin D intake may benefit those looking to support their cardiovascular health and manage hypertension effectively. Incorporating vitamin D-rich foods into the diet, engaging in safe sun exposure, and considering supplementation under the guidance of a healthcare provider can help individuals achieve optimal vitamin D levels and potentially enhance blood pressure management.
Determining the Optimal Dosage of Vitamin D for Blood Pressure Control
Finding the appropriate dosage of vitamin D for blood pressure control depends on individual health needs and current vitamin D levels. For most adults, the recommended amount is 600 to 800 IU per day. Some individuals may require higher amounts to achieve healthy blood levels. Consulting with a healthcare provider can help determine the best dose for your specific situation.
Various factors affect vitamin D requirements, including age, body weight, geographical location, and lifestyle habits. Individuals living in areas with limited sunlight exposure are at a higher risk of deficiency and may benefit from taking a supplement. A healthcare provider can assess your needs and recommend a dose that aligns with your health profile.
It is crucial to note that excessive vitamin D intake can lead to toxicity, resulting in elevated calcium levels and potential health complications. Hence, monitoring vitamin D levels through blood tests and collaborating with healthcare professionals is essential to ensure safety and efficacy. Individuals can take proactive steps to support their cardiovascular health and potentially reduce their risk of hypertension by focusing on achieving optimal vitamin D levels. Finding the right balance is key to reaping the benefits of this essential nutrient.
Identifying Dietary Sources of Vitamin D
Vitamin D can be obtained from various dietary sources, making it accessible for individuals seeking to boost their intake. Fatty fish, such as salmon, mackerel, and sardines, are excellent sources of vitamin D. Additionally, fortified foods, including dairy products, plant-based milk alternatives, and breakfast cereals, can provide significant amounts of this vital nutrient.
Sunlight exposure also plays a crucial role in obtaining vitamin D. When sunlight interacts with the skin, the body synthesizes vitamin D. This emphasizes the importance of outdoor time, especially during sunny months. However, several factors can diminish vitamin D production, including geographical location, skin pigmentation, and sunscreen usage. Consequently, some individuals may need to obtain vitamin D from food or supplements instead.
Supplements can be an effective solution for those unable to secure sufficient vitamin D through dietary means or sunlight exposure. Vitamin D3 (cholecalciferol) is generally regarded as the most effective form for increasing blood levels of vitamin D. When selecting supplements, opting for reputable brands that undergo third-party testing can assure quality and safety.
Incorporating a combination of dietary sources, sunlight exposure, and supplementation can help individuals achieve and maintain optimal vitamin D levels. This proactive approach may support overall health and potentially contribute to improved blood pressure management.
Reviewing Clinical Studies on Vitamin D and Hypertension
Researchers have reviewed numerous studies regarding vitamin D supplements and blood pressure. They found a slight decrease in pressure for some groups. Individuals with diabetes, low vitamin D levels, or short supplementation periods (under 20 weeks) experienced the best outcomes. In these cases, both systolic and diastolic blood pressure exhibited slight reductions. Nevertheless, not everyone benefitted; individuals with healthy vitamin D levels or those on long-term supplementation displayed minimal or no changes.
The results from research on vitamin D and blood pressure indicate promising trends, but not all studies demonstrate a clear connection. Variations in study designs, dosage used, and participant characteristics may elucidate these mixed results. As research progresses, it remains crucial to stay updated. New findings may redefine the role of vitamin D in managing high blood pressure. Consulting a healthcare provider can help you determine if and how to incorporate it into your health strategy. Vitamin D supports many aspects of overall health and may also aid in blood pressure regulation. Ensuring adequate intake through dietary sources, safe sun exposure, or supplementation can positively impact overall well-being and heart health.
Frequently Asked Questions About Blood Pressure Management
Which supplements are most effective for managing high blood pressure?
Some of the most effective supplements for controlling high blood pressure include magnesium, Potassium, omega-3 fatty acids, and Coenzyme Q10. These nutrients can support cardiovascular health and contribute to better blood pressure regulation.
How does magnesium contribute to lower blood pressure?
Magnesium helps to relax blood vessels and improve blood flow, leading to reduced blood pressure levels. Adequate magnesium intake is associated with a lower risk of hypertension.
What is potassium's role in regulating blood pressure?
Potassium helps counteract the effects of sodium in the body, promoting relaxation of blood vessel walls and lowering blood pressure. A diet rich in potassium can greatly benefit individuals with hypertension.
Are there risks associated with using supplements for high blood pressure?
Yes, certain supplements can interact with medications or cause side effects. It’s crucial to consult a healthcare provider before beginning any supplementation to ensure safety and effectiveness.
What is the recommended dosage of omega-3 fatty acids for blood pressure control?
Typical dosages of omega-3 supplements range from 1,000 to 4,000 mg per day. However, it is essential to consult a healthcare provider to determine the most suitable dosage tailored to individual needs.
Can garlic supplements effectively lower blood pressure?
Yes, garlic supplements, particularly those containing aged garlic extract, have shown potential benefits for lowering blood pressure due to their active compound, allicin. How does Coenzyme Q10 contribute to blood pressure management?
Coenzyme Q10 is an antioxidant that may help lower blood pressure by enhancing endothelial function and reducing oxidative stress within the body.
What is the recommended daily intake of vitamin D?
The recommended dietary allowance (RDA) for vitamin D in adults is 600 to 800 IU per day. However, individual requirements may vary, so it’s essential to consult a healthcare provider for personalised recommendations.
Can lifestyle changes alone effectively manage high blood pressure?
For many individuals, lifestyle changes such as a balanced diet, regular exercise, and stress management can effectively control high blood pressure without the need for medication. However, some individuals may still require medication for optimal management.
Is it safe to take multiple supplements for blood pressure management?
Taking multiple supplements can be safe, but it’s essential to consult a healthcare provider to ensure there are no interactions and that the combination is suitable for individual health needs.
Connect with us on Facebook!
The Article: Essential Supplements for Managing High Blood Pressure appeared first on https://janestevensnutrition.com
The Article: Essential Supplements for High Blood Pressure Management appeared first on https://janestevens.net
The Article High Blood Pressure Management with Essential Supplements Was Found On https://limitsofstrategy.com
The Article Essential Supplements for Managing High Blood Pressure First Appeared ON
: https://ad4sc.com

This is such an important topic. I’ve definitely noticed how easy it is to overlook blood pressure management until something alarming happens. My family has a history of hypertension, and I’ve recently started tracking my own readings regularly. It’s made me more aware not just of the numbers but also of how lifestyle factors like diet and stress play a role.