In-Depth Analysis of Blood Test Incubators for Improved Diagnostic Precision
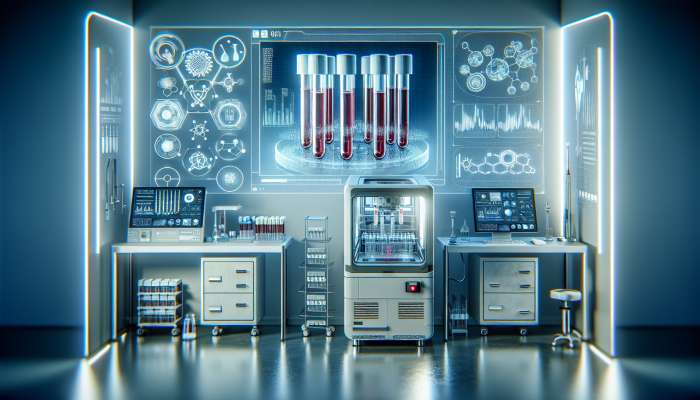
Understanding the Critical Role of Blood Test Incubators in Clinical Laboratories

A blood test incubator serves as a crucial component in the modern laboratory ecosystem, providing an essential environment for blood samples during diagnostic evaluations. These sophisticated machines are meticulously designed to uphold specific temperature and humidity parameters, both of which are indispensable for ensuring the accuracy and reliability of diagnostic outcomes. If incubation conditions are not adequate, it can severely compromise blood sample integrity, leading to erroneous test results that may endanger patient care. By consistently regulating these environmental factors, blood test incubators play a significant role in mitigating risks associated with temperature fluctuations, contamination, and other unpredictable variables that could disrupt vital biochemical reactions necessary for accurate diagnostics.
In the UK, healthcare professionals place immense reliance on these incubators for blood tests, which support various diagnostic procedures, including serology, haematology, and culture tests. The performance of a blood test incubator can profoundly influence the diagnostic workflow, underscoring its vital importance in clinical settings. Therefore, it is imperative for laboratories to invest in high-quality incubators that meet the rigorous standards set forth by regulatory authorities. This investment ensures the delivery of accurate and reproducible results, which are essential for effective patient management and treatment strategies.
Examining the Diverse Types of Blood Test Incubators Available in the Market
Blood test incubators come in an array of types, each meticulously crafted to meet specific testing needs and adapt to various laboratory settings. Understanding these different types can significantly aid laboratories in selecting the most appropriate equipment tailored to their operational requirements. For example, stationary incubators are robust units typically utilized in larger laboratory environments, providing ample capacity for high-throughput testing. These models often feature advanced systems for temperature and humidity control, ensuring optimal conditions are consistently maintained throughout the incubation time.
In contrast, portable incubators offer exceptional flexibility, allowing healthcare professionals to effortlessly transport samples between diverse locations such as clinics or field hospitals. This adaptability proves especially invaluable in emergency situations where rapid testing is essential. The choice between these two types largely depends on the laboratory's specific requirements, the volume of tests conducted, and logistical considerations. By choosing the appropriate incubator type, laboratories can markedly enhance their overall efficiency and effectiveness in performing blood tests.
The Vital Importance of Blood Test Incubators in Medical Diagnostics
The significance of a blood test incubator in the realm of medical diagnostics cannot be overstated. These devices are integral in preserving the viability of blood samples, which is critical for obtaining accurate test results. The incubation process ensures that samples remain in a stable environment, free from external contaminants that could jeopardize results. This dependability is essential for diagnosing a wide range of medical conditions, from infectious diseases to chronic illnesses.
In the UK, the healthcare system strongly emphasizes the need for precise diagnostics, as these results can directly influence treatment strategies and patient outcomes. Incorporating incubators into blood testing aligns with broader healthcare goals aimed at enhancing patient care through accurate and timely diagnostics. Furthermore, by adhering to regulations established by the UK's National Health Service (NHS) and other governing bodies, laboratories can ensure their practices meet the high standards necessary to maintain patient safety and the quality of care provided.
Key Steps for Setting Up Your Blood Test Incubator Effectively
Choosing the Right Location and Environmental Factors for Optimal Performance
The placement of a blood test incubator is a critical factor that greatly impacts its operational efficiency. Selecting the appropriate environment within the laboratory is vital, as extreme heat, cold, or humidity can negatively affect the incubation process. Ideally, incubators should be situated in a temperature-controlled area, protected from direct sunlight, drafts, or any sources of temperature fluctuations. This careful positioning guarantees that samples are consistently exposed to optimal conditions, thus enhancing the reliability of test outcomes.
In the UK, many laboratories are thoughtfully designed with dedicated spaces for sample processing, which aids in streamlining workflows and improving efficiency. It's also essential to consider additional factors, such as the stability of the electrical supply and ensuring convenient access to the incubator for routine inspections and maintenance. Additionally, situating the incubator near other vital laboratory equipment can enhance operational efficiency, enabling technicians to transition smoothly between tasks while safeguarding sample integrity.
Calibration Techniques and Initial Settings for Optimal Functionality
Calibrating your blood test incubator is a crucial procedure that ensures it operates at peak performance levels. This process typically entails adjusting the temperature and humidity settings according to the specific requirements of the tests being conducted. Most incubators include user manuals offering detailed guidance on the calibration process. However, having a comprehensive understanding of the specific parameters required for various blood tests is essential to guarantee optimal functionality.
Once calibration is complete, establishing the initial conditions before introducing any samples into the incubator is vital. This involves confirming that the incubator has reached the desired temperature and humidity levels, using precise measuring instruments for accuracy. Regular calibration of the unit should be performed, especially following any significant adjustments, to ensure that your blood test incubator usage remains reliable and efficient throughout its operational lifespan.
Ensuring Regulatory Compliance and Safety in Laboratory Operations
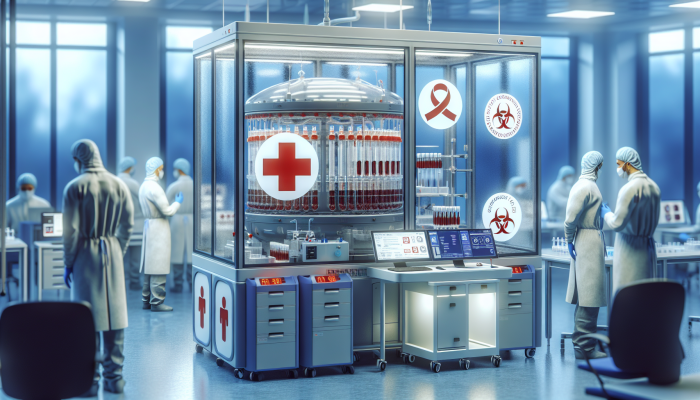
It is essential that your blood test incubator complies with health and safety regulations within the UK laboratory environment. Adhering to the standards set by the Care Quality Commission (CQC) and the Health and Safety Executive (HSE) is crucial for maintaining operational integrity and protecting laboratory personnel. This includes proper setup, ongoing maintenance, and operational protocols for the incubator, as well as training staff on best practices for safely and effectively handling biological materials.
Conducting regular risk assessments is vital for identifying potential hazards associated with the use of the incubator. This may involve evaluating the electrical safety of the unit and ensuring it is equipped with adequate safety features, such as alarms that alert users of any temperature deviations or power outages. By prioritizing safety and regulatory compliance, laboratories can cultivate a culture of accountability and professionalism, ultimately enhancing patient care outcomes.
Implementing Effective Cleaning and Maintenance Protocols
Routine maintenance and thorough cleaning of blood test incubators are crucial for preventing contamination and ensuring long-term operational efficiency. A comprehensive cleaning schedule should be established, detailing strict protocols for daily, weekly, and monthly tasks. This includes disinfecting internal surfaces, inspecting for signs of wear and tear, and confirming that all components are functioning as intended.
Laboratory technicians must be trained to promptly identify and address any potential issues. This proactive approach not only extends the lifespan of the incubator but also protects the integrity of blood samples. By integrating these maintenance routines into the laboratory's standard operating procedures, facilities can uphold the quality of their testing processes, ensuring reliable diagnostic outcomes for patients.
Maximising the Efficiency of Blood Test Incubators
Establishing Reliable Daily Operational and Maintenance Guidelines
Operating a blood test incubator requires a comprehensive understanding of daily procedures to guarantee optimal performance. This includes conducting routine checks of temperature and humidity levels and ensuring all settings remain consistent with established protocols tailored for specific tests. Technicians should diligently maintain a log of these checks, allowing them to identify any patterns or fluctuations that may warrant further investigation and corrective actions.
Additionally, daily maintenance should incorporate visual inspections of the unit to detect any signs of malfunction or damage. Any unusual sounds or indicators should be reported immediately to prevent disruptions in testing schedules. By fostering a culture of diligence and meticulous attention to detail, laboratories can maximise the effectiveness of their blood test incubator usage and ensure that sample integrity is consistently upheld.
Proactively Tackling Common Incubator Challenges
Every laboratory may encounter occasional challenges with their blood test incubators, making effective troubleshooting an essential skill for laboratory personnel. Common issues can include temperature fluctuations, humidity discrepancies, and equipment malfunctions. Quickly identifying these problems is essential to minimise their impact on testing procedures and preserve sample integrity.
For instance, if the temperature deviates from the desired range, technicians should first verify the calibration settings, followed by checking the incubator's door seal and electrical connections for any faults. Proper training in troubleshooting techniques equips staff to respond effectively to these situations, reducing downtime and ensuring that blood samples remain uncompromised. Regular training sessions can greatly enhance problem-solving skills and improve the overall efficiency of the laboratory's operations.
Utilising Data Logging and Monitoring for Enhanced Quality Assurance
In today's data-driven landscape, the ability to monitor and log incubation conditions is vital for laboratories conducting blood tests. Numerous modern incubators are equipped with advanced data logging capabilities that enable laboratory personnel to track temperature and humidity levels over extended periods. This technology not only aids in maintaining optimal conditions but also serves as essential documentation for compliance and quality control purposes.
Monitoring systems can generate alerts when conditions deviate from pre-set parameters, allowing for immediate corrective actions to be taken. By maintaining accurate records of incubation conditions, laboratories can substantiate their compliance with regulatory standards, which is crucial for audits and inspections. By adopting data-driven practices, laboratories can enhance the reliability of blood tests and bolster their reputation for delivering quality and precision in diagnostics.
Maintaining Optimal Temperature and Humidity Control
Achieving the correct temperature and humidity levels is fundamental for the successful incubation of blood samples. Each type of blood test may have specific requirements dictating optimal incubation conditions. For instance, certain cultures may thrive at elevated humidity levels, while others may necessitate stringent temperature control to prevent degradation.
Laboratories should invest in high-quality sensors and control systems that facilitate precise adjustments to these environmental factors. Regular calibration of these sensors is crucial to ensure their accuracy and reliability. By maintaining stable temperature and humidity levels, laboratories not only enhance the reliability of test results but also optimise the overall workflow, minimising the likelihood of retesting due to sample failure.
Establishing Robust Safety Protocols and Emergency Preparedness
Implementing strong safety protocols is essential for the secure operation of blood test incubators. Laboratory staff should receive comprehensive training in emergency procedures, including response plans for power outages, equipment failures, or exposure to hazardous materials. Regular drills can ensure that personnel are well-prepared to respond swiftly and effectively in emergencies, protecting both samples and staff members.
Furthermore, all laboratory personnel must be familiar with the specific safety features of the incubator, including automatic shut-off systems or alarms that alert users to temperature deviations. By fostering a culture of safety and preparedness, laboratories can significantly mitigate the risks associated with blood test incubators, ultimately enhancing the well-being of both staff and patients alike.
Implementing Best Practices for Blood Sample Incubation
Thorough Sample Preparation for Accurate Test Outcomes
The effective preparation of blood samples before incubation is critical for ensuring accurate test results. This process includes careful handling of samples to prevent contamination and degradation. Laboratory technicians must adhere to stringent protocols for collecting, processing, and storing blood samples to maintain their integrity throughout the testing procedure.
Utilising sterile equipment and following aseptic techniques are foundational aspects of this preparation phase. Additionally, blood samples should be meticulously labelled with essential information, including the patient’s details, type of test, and date of collection. This meticulous attention to detail significantly reduces the likelihood of errors and ensures that the samples can be traced back to their origin, a vital factor in maintaining quality control and safeguarding patient safety.
Comprehending Incubation Time and Temperature Requirements
Different blood tests have unique requirements regarding incubation time and temperature. Familiarity with these specifications is crucial for laboratory personnel to optimise the accuracy of test results. For example, culture tests may necessitate extended incubation times at specific temperatures to allow pathogens to proliferate adequately, while other tests may require rapid processing to maintain sample viability.
Laboratories should establish clear guidelines for each test type, detailing the precise incubation conditions required. Regular training sessions can help keep staff informed about these protocols, ensuring consistency in testing practices. By strictly adhering to these guidelines, laboratories can significantly enhance the reliability of their results, ultimately improving patient care and outcomes.
Strategies for Minimising Contamination Risks During Incubation
Preventing contamination during the incubation of blood samples is paramount for obtaining accurate test results. Laboratory personnel must implement stringent protocols to minimise the risk of cross-contamination, which can lead to erroneous findings. This includes employing proper handling techniques, utilising sterile instruments, and ensuring thorough cleaning of both the interior and exterior of the incubator.
Designating specific areas for blood sample processing and ensuring that all equipment is regularly disinfected further mitigates contamination risks. Training staff to recognise signs of contamination can also facilitate early detection and intervention. By prioritising contamination prevention, laboratories can uphold the integrity of their blood test incubator usage and confidently deliver high-quality diagnostics.
Investigating Advanced Features and Technologies in Blood Test Incubators
Utilising Automated Systems for Enhanced Laboratory Efficiency
The advent of automated blood test incubators represents a significant advancement in laboratory technology. These sophisticated systems are engineered to streamline the incubation process, resulting in increased efficiency and accuracy in testing. By automating temperature and humidity adjustments, laboratories can considerably diminish the potential for human error, leading to more reliable outcomes.
Automated systems frequently feature advanced monitoring capabilities, allowing for real-time data tracking and immediate alerts should conditions deviate from optimal ranges. This not only enhances operational efficiency but also ensures that laboratories comply with stringent health standards. Investing in these state-of-the-art solutions can significantly improve blood test incubator usage and enhance patient care delivery.
Connectivity Features and Data Integration for Streamlined Laboratory Operations
Modern blood test incubators increasingly incorporate connectivity features that facilitate seamless integration with laboratory management systems. This connectivity improves data management, enabling laboratories to effectively track and analyse incubation conditions. By integrating incubator data with other laboratory processes, such as sample tracking and reporting, labs can streamline workflows and reduce the potential for errors.
Data integration allows the generation of comprehensive reports for audits and regulatory compliance, demonstrating a commitment to quality assurance. The ability to access real-time data remotely empowers laboratory personnel to make informed decisions, further optimising the incubation process. By embracing these technological advancements, laboratories can significantly elevate their operational efficiency and improve diagnostic accuracy.
Anticipating Future Trends in Incubation Technology
The field of blood test incubation technology is rapidly evolving, with several emerging trends poised to revolutionise laboratory practices. Innovations in smart technology, including artificial intelligence and machine learning, are anticipated to enhance how laboratories monitor and control incubation conditions. These advancements may predict when maintenance is necessary or automatically adjust settings based on real-time data inputs.
Sustainability is also becoming a focal point in laboratory design, with eco-friendly incubators being developed that consume less energy and produce minimal waste. These advancements not only benefit the environment but also assist laboratories in reducing operational costs. By staying ahead of these trends, laboratories can ensure their continued competitiveness in delivering high-quality diagnostic services.
Implementing Enhanced Security Features for Data Protection
In the current digital landscape, protecting sensitive patient data is of utmost importance for laboratories. Enhanced security measures must be integrated into blood test incubators, particularly those equipped with connectivity features. This includes robust encryption protocols, user authentication systems, and regular software updates to safeguard against potential breaches.
Compliance with data protection legislation, such as the UK General Data Protection Regulation (GDPR), is crucial for maintaining the trust of patients and stakeholders alike. Training laboratory personnel on data security best practices further strengthens the overall security framework. By prioritising data security, laboratories can ensure that their blood test incubator usage aligns with regulatory standards while protecting patient confidentiality and trust.
Advancing Energy Efficiency and Sustainability in Laboratory Practices
The growing emphasis on sustainability within laboratory environments has led to an increasing demand for energy-efficient blood test incubators. These innovations not only contribute to reducing the carbon footprint of healthcare facilities but also result in significant cost savings over time. Energy-efficient designs often incorporate advanced insulation materials and intelligent temperature control systems to minimise energy consumption without compromising performance.
Moreover, laboratories adopting these eco-friendly practices can enhance their reputation as responsible entities committed to environmental stewardship. By investing in sustainable technologies, facilities can align with broader healthcare initiatives aimed at promoting sustainability within the sector. Embracing these energy-efficient solutions ultimately improves the effectiveness of blood test incubator usage while contributing to a healthier and more sustainable planet.
Emphasising Training and Education for Laboratory Personnel
Establishing Comprehensive Training Programmes for Staff
Developing comprehensive training programmes for laboratory personnel is essential for ensuring the effective use and maintenance of blood test incubators. Staff should receive thorough instruction in operational protocols, safety measures, and troubleshooting techniques associated with these essential devices. Such training not only enhances individual capabilities but also fosters a culture of excellence within the laboratory environment.
Regular training sessions should also be conducted to cover updates on new technologies and methodologies, ensuring that staff remain knowledgeable about best practices in blood testing. By investing in ongoing education, laboratories can cultivate a proficient workforce capable of optimising blood test incubator usage and contributing to improved patient outcomes.
Encouraging Continuous Education for Laboratory Professionals
The field of medical diagnostics is continually evolving, making ongoing education a vital aspect for laboratory personnel working with blood test incubators. Numerous resources, including online courses, workshops, and conferences, provide opportunities for professionals to expand their knowledge and stay current with industry developments. Engaging in these educational pursuits can significantly enhance skills, particularly in data management, laboratory safety, and technology integration.
Participation in ongoing education also fosters networking opportunities with other professionals in the field, facilitating the exchange of innovative ideas and best practices. By promoting a culture of lifelong learning, laboratories can ensure their personnel are equipped with the most up-to-date knowledge and techniques, ultimately leading to more effective blood test incubator usage and improved diagnostics.
Recognising the Importance of Certification and Accreditation in Laboratories
Certification and accreditation are crucial components in maintaining high standards within blood testing laboratories. Compliance with recognised standards, such as ISO 15189, ensures that laboratories adhere to best practices in quality management and diagnostic accuracy. Achieving accreditation necessitates thorough documentation of processes, including the proper usage and maintenance of blood test incubators.
Regular assessments and audits are conducted to verify compliance with these standards, underscoring the importance of maintaining stringent quality control measures. By prioritising certification and accreditation, laboratories can enhance their credibility and demonstrate a commitment to delivering high-quality diagnostic services, further emphasising the significance of effective blood test incubator usage.
Implementing Safety Training and Protocols in Laboratory Environments
Safety training is a critical aspect of laboratory education, particularly concerning the operation of blood test incubators. Personnel should receive training on the specific hazards associated with the incubator, as well as the proper procedures for handling biological materials. This includes understanding emergency protocols related to equipment malfunctions, power failures, or exposure incidents.
Conducting regular safety drills can reinforce these protocols, ensuring that staff are well-prepared to respond effectively to emergencies. By incorporating safety training into the laboratory culture, facilities can mitigate risks associated with blood test incubators, thereby enhancing both staff safety and the reliability of diagnostic processes.
Common Questions Regarding Blood Test Incubators
What are the primary functions of blood test incubators?
Blood test incubators are specifically designed to maintain optimal temperature and humidity conditions for blood samples during diagnostic testing, ensuring the accuracy and reliability of test results.
How can I determine the most suitable blood test incubator for my laboratory?
Selecting the right blood test incubator depends on your laboratory's specific requirements, including the volume of tests performed, the types of samples processed, and the available space. Evaluate the advantages of portable versus stationary models based on your operational needs.
What maintenance tasks are essential for blood test incubators?
Regular maintenance includes cleaning both the interior and exterior surfaces, calibrating temperature and humidity sensors, and conducting routine checks for signs of malfunction or wear.
How frequently should I calibrate my blood test incubator?
Calibration should be performed regularly, ideally before initial use and periodically thereafter, or whenever significant adjustments are made to the settings.
What are the risks of not using a blood test incubator?
Neglecting to utilise a blood test incubator can compromise sample integrity, resulting in inaccurate test results, misdiagnosis, and potentially harmful consequences for patient care.
Can blood test incubators be used for other types of biological samples?
While blood test incubators are primarily designed for blood samples, certain models may be suitable for other biological materials, provided they meet the necessary conditions required for those samples.
What key features should I consider when selecting a blood test incubator?
Key features to assess include precise temperature and humidity controls, data logging capabilities, alarm systems for deviations, and ease of cleaning and maintenance procedures.
Is training necessary for the effective operation of a blood test incubator?
Yes, comprehensive training is vital to ensure the safe and effective operation, maintenance, and troubleshooting of blood test incubators, ultimately safeguarding the integrity of samples.
How can I mitigate contamination risks in a blood test incubator?
Preventing contamination necessitates strict adherence to aseptic techniques, regular cleaning of the incubator, and ensuring that all instruments used are sterile and handled properly.
What impact does automation have on blood test incubators?
Automation enhances the efficiency and accuracy of blood test incubators by minimising human error, facilitating real-time monitoring, and improving overall laboratory workflows.
Connect with us on Facebook!
This Article Was First Found On https://bloodtest.co.uk
The Article Blood Test Incubator Use: Essential Insights and Tips Was Found On https://limitsofstrategy.com
The Article Blood Test Incubator: Key Insights and Essential Tips First Appeared ON
: https://ad4sc.com